
According to a British American study, the pathogens that cause chickenpox and herpes together can lead to dementia.
Just a few weeks ago, a scientific scandal involving seemingly fake studies on the development of Alzheimer’s rocked research in this important area. The processes that lead to changes in the brain are still only partially understood; What drives them remains a mystery. Researchers from Tufts University in Massachusetts (USA) and Oxford University (England) added one piece of the puzzle – or more – to answer this question. The US-British team reinforced suspicions that the varicella-zoster and herpes simplex viruses play a role – and deciphered a mechanism by which pathogens cause brain damage.
According to the study, varicella-zoster virus (VZV), which causes chickenpox and herpes zoster, can activate herpes simplex virus to “initiate the early stages of Alzheimer’s disease,” according to a statement from Tufts University. The results were published in the Journal of Alzheimer’s Disease.
The herpes simplex and varicella zoster viruses are among the most common of all. Both belong to the herpes virus family, after an acute illness the body remains “dormant” and can be reactivated; Characteristics that may be of critical importance to the development of Alzheimer’s disease. It is estimated that 95 percent of people develop varicella-zoster before the age of 20. In most cases, this leads to chickenpox, and later reactivation of the virus to painful shingles (herpes zoster).
According to the World Health Organization, about 3.7 billion people under the age of 50 are infected with HSV-1, one of the most common forms of herpes simplex. HSV-1 causes uncomfortable blisters on the lips. He spends most of his time silently in the body without provoking any symptoms, lying dormant in neurons; Also in the brain. However, in the active state, HSV-1 viruses can lead to the accumulation of amyloid beta and tau proteins there, according to a Tufts University statement.
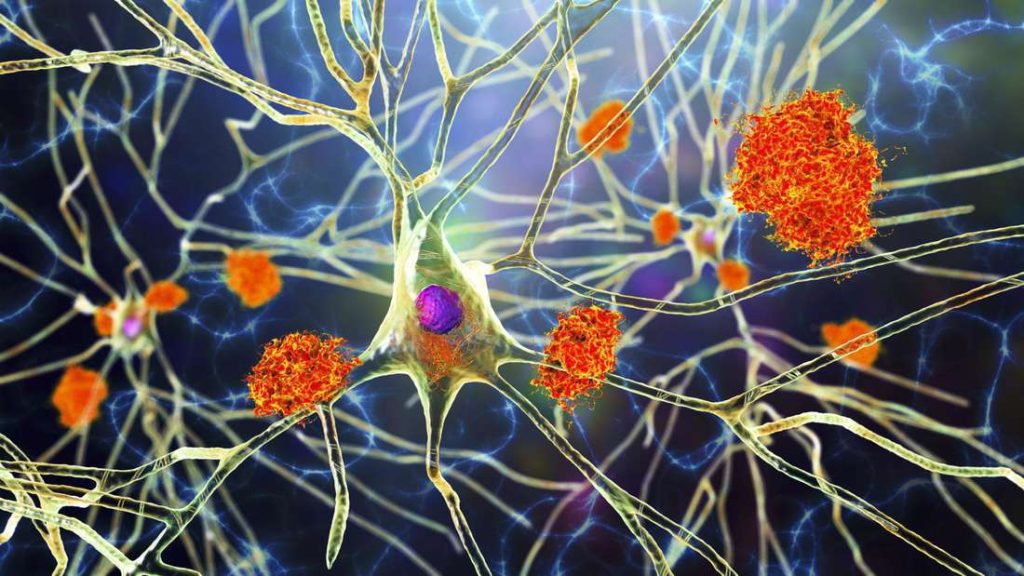
Both proteins undergo fatal changes in Alzheimer’s disease. For example, bits of amyloid beta proteins can clump together to form plaques and tau proteins can form twisted, elongated fibers called fibrils. However, how these processes relate and what exactly they do is not yet fully understood. The so-called purported studies centered around this set of questions.
The US-British research team now claims to have discovered that infection with the varicella-zoster virus sets in motion inflammatory processes, which in turn awaken dormant herpes simplex viruses in the brain. The possibility of a link between herpes simplex viruses and Alzheimer’s disease has been debated for some time. Neuroscientist Ruth Itzaki of the University of Cambridge and Oxford University was among the first to raise and research this suspicion. She also participated in the current study.
“We know there is a link between HSV-1 and Alzheimer’s disease, and some have suggested that VZV may also be involved. But what we didn’t know was the sequence of events that viruses create to initiate the disease,” says David Kaplan, chair of the Department of Biomedical Engineering at the College of Medicine. Tufts Engineering.” We believe we now have evidence of these events.”
In their study, the researchers used a 3D model of human tissue culture that simulated the brain. They reproduced their skeletons in a small, six-millimeter-wide sponge made of silk protein and collagen. In turn, they filled the sponge with neural stem cells, which become functional neurons capable of transmitting signals in a network — just as they would in a real brain.
Researchers have found that neurons implanted in brain tissue can develop varicella zoster. However, this alone did not lead to the formation of amyloid beta and tau proteins, which are central to Alzheimer’s disease. However, if the neurons contained the dormant HSV-1, exposure to varicella-zoster reactivated it – which in turn led to a ‘dramatic increase’ in tau and beta-amyloid proteins. The result: the nerve signals slowed down.
“It’s a double whammy of two common and usually harmless viruses, but laboratory studies suggest that they can cause problems when new exposure to VZV awakens dormant HSV-1,” explains Dana Kearns of Tufts University.
The researchers also noted that samples infected with varicella-zoster began producing cytokines. Cytokines are proteins involved in inflammatory processes – in fact, inflammation caused by infection can be observed in brain tissue. It is possible, according to David Kaplan, that this inflammation led to the activation of dormant herpes simplex viruses in the brain — and to greater inflammation. Researchers theorize that the risk of developing Alzheimer’s disease is primarily increased by repeated activation of herpes simplex in the brain. Vaccination against chickenpox can “significantly reduce”.
However, “other infections and other pathways can also lead to Alzheimer’s disease,” adds Dana Kearns. Interaction with risk factors such as head trauma, severe obesity and alcohol consumption can also be visualized. Coronavirus has also been suspected to be able to induce Alzheimer’s disease, but a causal relationship cannot be proven. A large study from Denmark noted that the risk of Alzheimer’s disease and Parkinson’s disease increased from six months to a year after infection, but this also applies to influenza and bacterial pneumonia. So some scientists suspected that the cause was less than the coronavirus itself and the inflammation associated with the infection.
The US-UK research team is now working on the idea that Sars-CoV-2 can reactivate both varicella-zoster and herpes simplex viruses in the body. It’s wise to keep this in mind, they write.






More Stories
Exploding Fireball: Find the meteorite fragments
Neuralink's competitor lets blind people see again with an implant
A huge meteorite has hit Earth – four times the size of Mount Everest