(Vienna, January 10, 2024) Because the cause of chronic inflammatory bowel diseases (IBD) such as Crohn's disease or ulcerative colitis is not yet known, treatment for those affected is currently aimed at alleviating the often uncomfortable symptoms. The discovery by a research team at MedUni Vienna that the trigger of inflammatory bowel disease (IBD) can be found on the surface of intestinal epithelial cells provides a new potential starting point for the development of therapeutic measures. The results of the study were recently published in the specialized journal EMBO Reports.
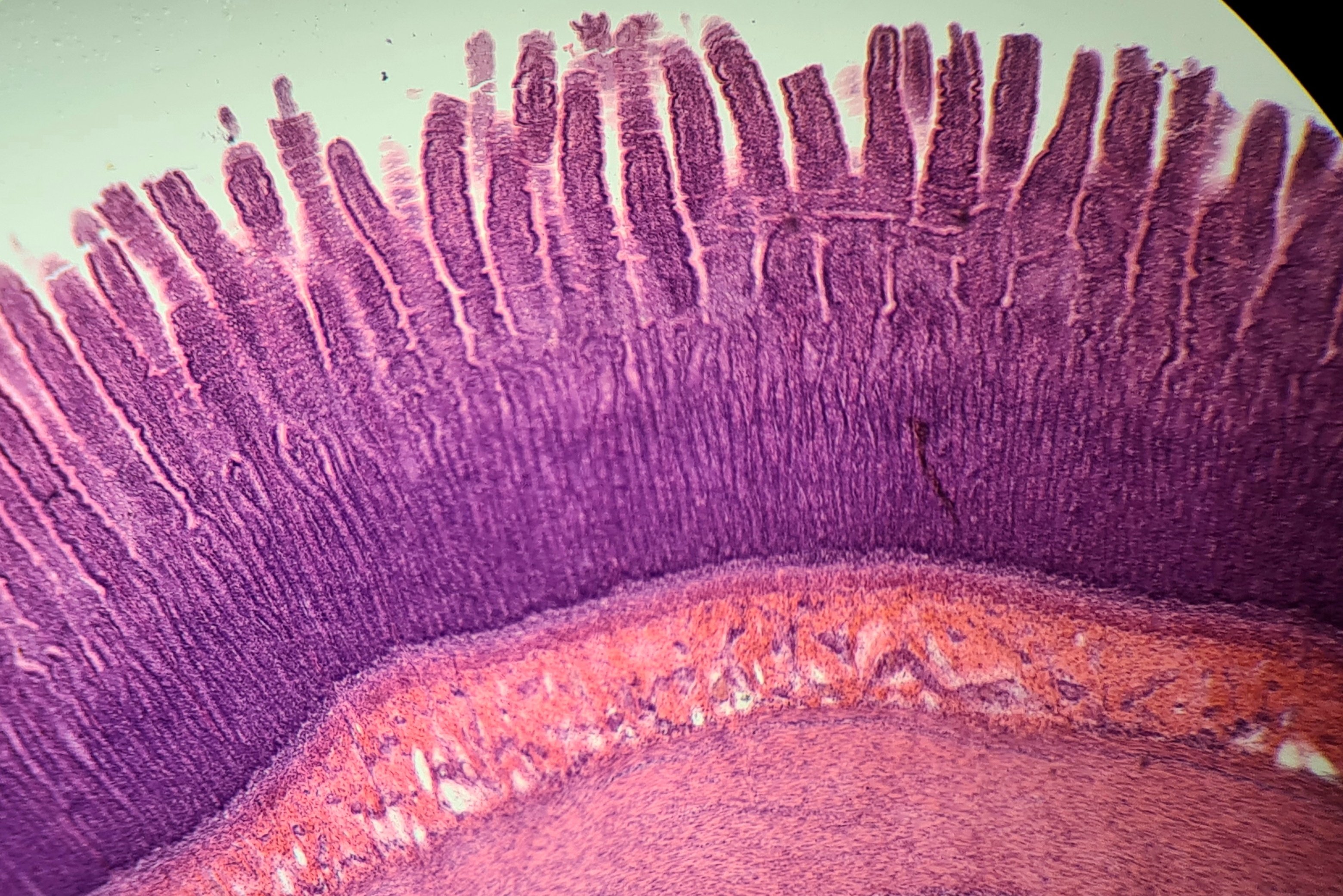
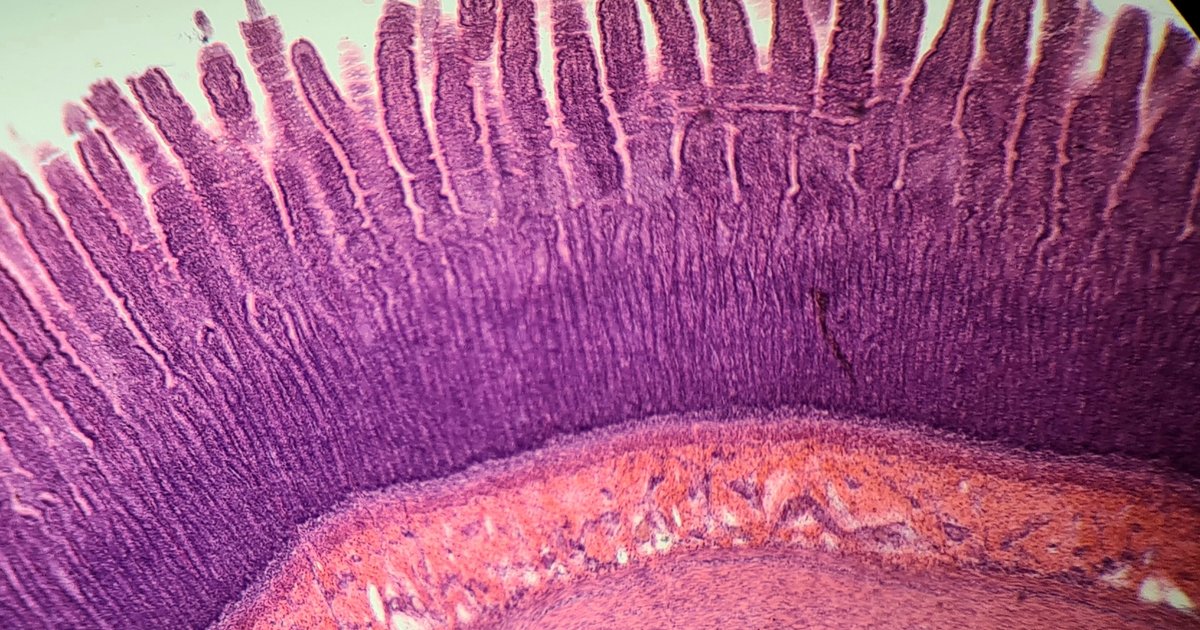
In their experiments, the research group led by Bernadette Modell and Robert Everle from the Center for Cancer Research (ZKF) and the Comprehensive Cancer Center (CCC) at MedUni Vienna were able to show for the first time that certain changes in brush borders of intestinal epithelial cells can be linked to the development of inflammatory bowel disease (IBD). Brush borders consist of dense, finger-shaped projections (microvilli) on the surface of intestinal epithelial cells, which are the cells of the outer layer of the intestine. Microvilli are connected to each other by a protein complex (intermicrobial adhesion complex = IMAC), which is responsible for the organized structure of the brush border.
Enhancing the production of some proteins
It has been known for some time that a certain IMAC protein (CDHR5) is present at low levels in people with inflammatory bowel disease. In order to explore previously unknown links, the research team created a mouse model in which CDHR5 was missing. As seen by electron microscopy, the brush border microvilli in these mice appeared shorter and quite disordered, like shaggy hair. “But this alone did not lead to the penetration of harmful bacteria and the development of intestinal infection,” says Bernadette Modell, lead author of the study. IBD only occurred after the protective mucus layer over intestinal epithelial cells became permeable as part of the experiment.
“It was found that decreased or lost IMAC protein and associated regulatory deficits in the brush border, as well as mucosal layer permeability, may be a potential trigger for chronic inflammatory bowel disease,” says study leader Robert Everle, summarizing the findings. . Accordingly, active components that enhance the production of IMAC proteins in intestinal epithelial cells could represent a potential starting point for the development of a causal treatment for IBD.
The fact that unhealthy food high in fat is associated with the development of inflammatory bowel disease (IBD) can also be explained by the results of the present study, because this diet makes the mucus layer located at the brush border of intestinal epithelial cells more permeable. This may be especially critical for people with a family history of low CDHR5 production.
The research was carried out in close cooperation with colleagues from the Clinical Institute of Pathology and the University Clinic of Oral and Maxillofacial Surgery at MedUni Vienna as well as with partners from the University of Vienna.
Publication: EMBO Reports
Defects in microvilli tangles cause colitis and inflammatory bowel disease.
Bernadette Modell, Munira Awad, Daniela Zolanick, Irene Scharf, Katharina Schwertner,
Daniela Milovanovic, Doris Moser, Katie Schmidt, Petra Pejevac, Bela Hausmann, Dana Krause,
Thomas Mohr, Jasmine Svenka, Lukas Keener, Emilio Casanova, Gerald Timmelthaler,
Maria Sibelia, Sigurd Krieger, and Robert Everell
DOI 10.15252/ebr.202357084

“Total coffee aficionado. Travel buff. Music ninja. Bacon nerd. Beeraholic.”







More Stories
Coral Seeding: Artificial Insemination Makes Coral More Heat Tolerant
Fear, Anger, and Denial: How People Respond to Climate Change – Research
LKH Graz: Using radiation to combat heart arrhythmias